16.1 Reducing Disorder by Confronting It: Psychotherapy
Learning Objectives
- Outline and differentiate different types of care providers.
- Explain the behavioural and cognitive aspects of cognitive-behavioural therapy and how it is used to reduce psychological disorders.
Treatment for psychological disorders is provided in a wide variety of settings by practitioners who come from different backgrounds. For many people, their first interaction is with a family physician who may prescribe medication or refer the individual for further mental health services. The type of care the individual receives will depend on a number of factors, including the training and experience of the care provider and the theoretical and philosophical orientation of the care provider. In this section, we will consider some of the most common care providers.
Clinical psychologists have advanced degrees in clinical psychology, usually a master’s degree and a doctorate, with a clinical internship under the supervision of an established clinical psychologist. Thus, training takes several years after first earning a bachelor’s degree. Once the training is complete, the individual registers with a professional body, such as College of Psychologists in British Columbia, and is bound by a professional code of conduct. Some clinical psychologists specialize, for example, in the treatment of children or in specific disorders, such as schizophrenia. Clinical psychologists may work in private practice or be attached to a clinic, jail, rehabilitation centre, university, and so on. They may conduct individual, couples, family, and group therapy. They treat people with a variety of disorders and may work from one theoretical perspective, such as behaviourist, or they may use an eclectic array of techniques from several orientations. Clinical psychologists are not allowed to prescribe medication but may work in tandem with a physician. As well as treating people for psychological disorders or distress, clinical psychologists also assess cognitive functioning, and they provide help to people with physical conditions.
A psychiatrist is a physican who has completed a specialization in psychiatry. Psychiatrists and clinical psychologists do much of the same work; however, psychiatrists may prescribe medication and may be more likely to focus on biological treatments.
A counsellor is typically a care provider with a master’s degree in counselling psychology. Their work is to help people who feel challenged in some area of life, such as marriage or personal relationships, substance use, recovery from trauma, and so on. Professional organizations, such as the BC Association of Clinical Counsellors, oversee the registration of counsellors. Some counsellors attain doctorates and then become registered psychologists.
There are many other professions that provide care for psychological distress or mental illness, such as art therapists, clinical social workers, psychiatric nurses, and so on. It is also possible for people who are untrained in any type of therapy to call themselves a therapist or psychotherapist. This highlights the need for those seeking therapy to inquire about the education, training, and experience of the individual providing care.
Whatever therapist provides care, it is important that they explain the goals of therapy and agree on a course of action with the person seeking therapy. A successful therapeutic alliance maximizes the chance that therapy will be effective. While therapists differ in theoretical orientations, it is important for the therapist to be warm, non-judgmental, and empathic. Sometimes, finding a therapist who understands the cultural background can be important. For example, Indigenous Canadians may find it more comfortable and effective to seek therapy from a therapist who has a deep understanding of the complex intergenerational effects of colonization and genocide of Indigenous Peoples; this may include elders and traditional healers as cultural supports (National Inquiry into Missing and Murdered Indigenous Women and Girls, 2019).
One approach to treatment is psychotherapy, the professional treatment for psychological disorder through techniques designed to encourage communication of conflicts and insight. The fundamental aspect of psychotherapy is that the patient directly confronts the disorder and works with the therapist to help reduce it. Therapy includes assessing the patient’s issues and problems, planning a course of treatment, setting goals for change, the treatment itself, and an evaluation of the patient’s progress. Therapy is practised by thousands of psychologists and other trained practitioners in Canada, responsible for billions of dollars of the health budget.
To many people, therapy involves a patient lying on a couch with a therapist sitting behind and nodding sagely as the patient speaks. Though this approach to therapy, known as psychoanalysis, is still practised, it is in the minority. It is estimated that there are over 400 different kinds of therapy practised by people in many fields, and the most important of these are psychodynamic, humanistic, cognitive behavioural therapy, and eclectic (i.e., a combination of therapies).
Psychology in Everyday Life
Seeking treatment for psychological difficulties
Many people who would benefit from psychotherapy do not get it, either because they do not know how to find it or because they feel that they will be stigmatized and embarrassed if they seek help. The decision to not seek help is a very poor choice because the effectiveness of mental health treatments is well documented. No matter where a person lives, there are treatments available (Canadian Mental Health Association, 2013).
The first step in seeking help for psychological problems is to accept the stigma. It is possible that some of your colleagues, friends, and family members will know that you are seeking help, and some may at first think more negatively of you for it. However, you must get past these unfair and close-minded responses. Feeling good about yourself is the most important thing you can do, and seeking help may be the first step in doing so.
One question is how to determine if someone needs help. This question is not always easy to answer because there is no clear demarcation between normal and abnormal behaviour. Most generally, you will know that you or others need help when the person’s psychological state is negatively influencing their everyday behaviour, when the behaviour is adversely affecting those around the person, and when the problems continue over a period of time. Often people seek therapy as a result of a life-changing event — such as diagnosis of a fatal illness, an upcoming marriage or divorce, or the death of a loved one — but therapy is also effective for general depression and anxiety, as well as for specific everyday problems.
There are a wide variety of therapy choices, many of which are free. Begin in your school, community, or church by asking about community health or counselling centres and pastoral counselling. You may want to ask friends and family members for recommendations. You’ll probably be surprised at how many people have been to counselling and how many recommend it.
There are many therapists who offer a variety of treatment options. Be sure to ask about the degrees that the therapist has earned and about the reputation of the centre in which the therapy occurs. If you have choices, try to find a person or location that you like, respect, and trust. This will allow you to be more open, and you will get more out of the experience. Your sessions with the help provider will require discussing your family history, personality, and relationships, and you should feel comfortable sharing this information.
Remember that confronting issues requires time to reflect, energy to get to the appointments and deal with consequential feelings, and discipline to explore your issues on your own. Success at therapy is difficult, and it takes effort.
The bottom line is that going for therapy should not be a difficult decision for you. All people have the right to appropriate mental health care, just as they have a right to general health care. Just as you go to a dentist for a toothache, you may go to therapy for psychological difficulties.
Psychoanalysis and psychodynamic therapy
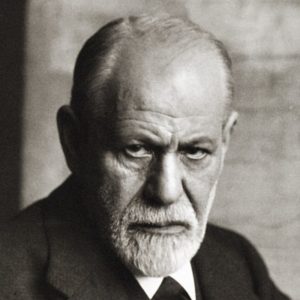
The earliest organized therapy for mental disorders was psychoanalysis. Made famous in the early 20th century by one of the best-known clinicians of all time, Sigmund Freud, this approach stresses that mental health problems are rooted in unconscious conflicts and desires. In order to resolve the mental illness, then, these unconscious struggles must be identified and addressed. Psychoanalysis often does this through exploring one’s early childhood experiences that may have continuing repercussions on one’s mental health in the present and later in life. Psychoanalysis is an intensive, long-term approach in which patients and therapists may meet multiple times per week, often for many years.
History of psychoanalytic therapy
Freud initially suggested that mental health problems arise from efforts to push inappropriate sexual urges out of conscious awareness (Freud, 1895/1955). Later, Freud suggested more generally that psychiatric problems are the result of tension between different parts of the mind: the id, the superego, and the ego. In Freud’s structural model, the id represents pleasure-driven unconscious urges (e.g., our animalistic desires for sex and aggression), while the superego is the semi-conscious part of the mind where morals and societal judgment are internalized (e.g., the part of you that automatically knows how society expects you to behave). The ego — also partly conscious — mediates between the id and superego. Freud believed that bringing unconscious struggles like these, where the id demands one thing and the superego another, into conscious awareness would relieve the stress of the conflict (Freud, 1920/1955), which became the goal of psychoanalytic therapy.
Although psychoanalysis is still practised today, it has largely been replaced by the more broadly defined psychodynamic therapy. This latter approach has the same basic tenets as psychoanalysis, but it is briefer, makes more of an effort to put clients in their social and interpersonal context, and focuses more on relieving psychological distress than on changing the person.
Techniques in psychoanalysis
Psychoanalysts and psychodynamic therapists employ several techniques to explore patients’ unconscious mind. One common technique is called free association. Here, the patient shares any and all thoughts that come to mind, without attempting to organize or censor them in any way. For example, if you took a pen and paper and just wrote down whatever came into your head, letting one thought lead to the next without allowing conscious criticism to shape what you were writing, you would be partaking in free association. The analyst then uses their expertise to discern patterns or underlying meaning in the patient’s thoughts.
Sometimes, free association exercises are applied specifically to childhood recollections. That is, psychoanalysts believe a person’s childhood relationships with caregivers often determine the way that person relates to others and predicts later psychiatric difficulties. Thus, exploring these childhood memories, through free association or otherwise, can provide therapists with insights into a patient’s psychological makeup.
Since we do not always have the ability to consciously recall these deep memories, psychoanalysts also discuss their patients’ dreams. In Freudian theory, dreams contain not only manifest, or literal, content but also latent, or symbolic, content (Freud, 1900/1955). For example, someone may have a dream that their teeth are falling out — the manifest content of the dream. However, dreaming that one’s teeth are falling out could be a reflection of the person’s unconscious concern about losing their physical attractiveness — the latent content of the dream. It is the therapist’s job to help discover the latent content underlying one’s manifest content through dream analysis.
In psychoanalytic and psychodynamic therapy, the therapist plays a receptive role, interpreting the patient’s thoughts and behaviour based on clinical experience and psychoanalytic theory. For example, if during therapy a patient begins to express unjustified anger toward the therapist, the therapist may recognize this as an act of transference. That is, the patient may be displacing feelings for people in their life (e.g., anger toward a parent) onto the therapist. At the same time, though, the therapist has to be aware of their own thoughts and emotions, because, in a related process called counter-transference, the therapist may displace their own emotions onto the patient.
The key to psychoanalytic theory is to have patients uncover the buried, conflicting content of their mind, and therapists use various tactics, such as seating patients to face away from them, to promote a freer self-disclosure. As a therapist spends more time with a patient, the therapist can come to view their relationship with the patient as another reflection of the patient’s mind.
Advantages and disadvantages of psychoanalytic therapy
Psychoanalysis was once the only type of psychotherapy available, but presently, the number of therapists practising this approach is decreasing around the world. Psychoanalysis is not appropriate for some types of patients, including those with severe psychopathology or intellectual disability. Further, psychoanalysis is often expensive because treatment usually lasts many years. Still, some patients and therapists find the prolonged and detailed analysis very rewarding.
Perhaps the greatest disadvantage of psychoanalysis and related approaches is the lack of empirical support for their effectiveness. The limited research that has been conducted on these treatments suggests that they do not reliably lead to better mental health outcomes (e.g., Driessen et al., 2010). Although there are some reviews that seem to indicate that long-term psychodynamic therapies might be beneficial (e.g., Leichsenring & Rabung, 2008), other researchers have questioned the validity of these reviews. Nevertheless, psychoanalytic theory was history’s first attempt at formal treatment of mental illness, setting the stage for the more modern approaches used today.
Humanistic therapies
Just as psychoanalysis is based on the personality theories of Freud and the neo-Freudians, humanistic therapy is a psychological treatment based on the personality theories of Carl Rogers and other humanistic psychologists. Humanistic therapy is based on the idea that people develop psychological problems when they are burdened by limits and expectations placed on them by themselves and others, and the treatment emphasizes the person’s capacity for self-realization and fulfillment. Humanistic therapies attempt to promote growth and responsibility by helping clients consider their own situations and the world around them and how they can work to achieve their life goals.
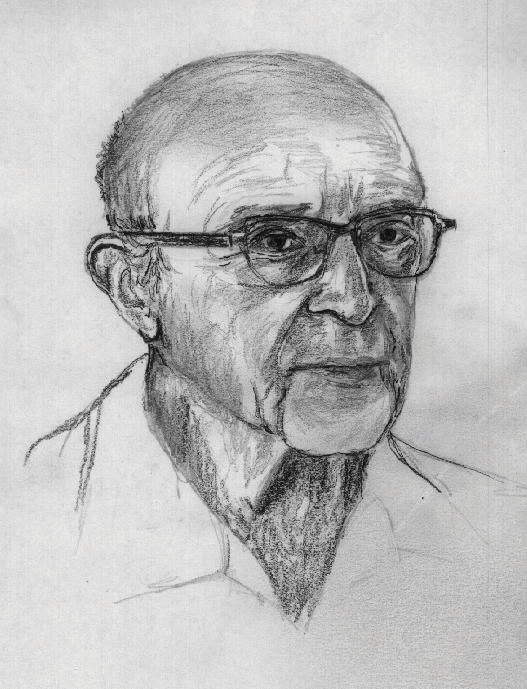
Carl Rogers (see Figure 16.3) developed person-centred (or client-centred) therapy, which is an approach to treatment in which the client is helped to grow and develop as the therapist provides a comfortable, nonjudgmental environment. In his book A Way of Being (1980), Rogers argued that therapy was most productive when the therapist created a positive relationship with the client — a therapeutic alliance. The therapeutic alliance is a relationship between the client and the therapist that is facilitated when the therapist is genuine (i.e., they create no barriers to free-flowing thoughts and feelings), when the therapist treats the client with unconditional positive regard (i.e., they value the client without any qualifications, displaying an accepting attitude toward whatever the client is feeling at the moment), and when the therapist develops empathy with the client (i.e., they actively listen to and accurately perceive the personal feelings that the client experiences).
The development of a positive therapeutic alliance has been found to be exceedingly important to successful therapy. The ideas of genuineness, empathy, and unconditional positive regard in a nurturing relationship in which the therapist actively listens to and reflects the feelings of the client is probably the most fundamental part of contemporary psychotherapy (Prochaska & Norcross, 2007).
Advantages and disadvantages of person-centred therapy
One key advantage of person-centred therapy (PCT) is that it is highly acceptable to patients. In other words, people tend to find the supportive, flexible environment of this approach very rewarding. Furthermore, some of the themes of PCT translate well to other therapeutic approaches. For example, most therapists of any orientation find that clients respond well to being treated with nonjudgmental empathy. The main disadvantage to PCT, however, is that findings about its effectiveness are mixed. One possibility for this could be that the treatment is primarily based on unspecific treatment factors. That is, rather than using therapeutic techniques that are specific to the patient and the mental problem (i.e., specific treatment factors), the therapy focuses on techniques that can be applied to anyone, such as establishing a good relationship with the patient (Cuijpers et al., 2012; Friedli, King, Lloyd, & Horder, 1997). Similar to how “one-size-fits-all” doesn’t really fit every person, PCT uses the same practices for everyone, which may work for some people but not others. Further research is necessary to evaluate its utility as a therapeutic approach.
Psychodynamic and humanistic therapies are recommended primarily for people suffering from generalized anxiety or mood disorders and for those who desire to feel better about themselves overall. However, the goals of people with other psychological disorders — such as phobias, sexual problems, and obsessive-compulsive disorder (OCD) — are more specific. A person with a social phobia may want to be able to leave their house, a person with a sexual dysfunction may want to improve their sex life, and a person with OCD may want to learn to stop letting their obsessions or compulsions interfere with everyday activities. In these cases, it is not necessary to revisit childhood experiences or consider our capacities for self-realization; we simply want to deal with what is happening in the present.
Cognitive behavioural therapy (CBT) is a structured approach to treatment that attempts to reduce psychological disorders through systematic procedures based on cognitive and behavioural principles. CBT is based on the idea that there is a recursive link among our thoughts, our feelings, and our behaviour. For instance, if we are feeling depressed, our negative thoughts (e.g., “I am doing poorly in my chemistry class”) lead to negative feelings (e.g., “I feel hopeless and sad”), which then contribute to negative behaviours, such as lethargy or lack of interest. When we or other people look at the negative behaviour, the negative thoughts are reinforced and the cycle repeats itself (A. T. Beck, 1976). Similarly, in panic disorder, a patient may misinterpret their feelings of anxiety as a sign of an impending physical or mental catastrophe (e.g., a heart attack), leading to an avoidance of a particular place or social situation. The fact that the patient is avoiding the situation reinforces the negative thoughts. Again, the thoughts, feelings, and behaviour amplify and distort each other.
CBT is a very broad approach that is used for the treatment of a variety of problems, including mood, anxiety, personality, eating, substance abuse, attention-deficit, and psychotic disorders. CBT treats the symptoms of the disorder (i.e., the behaviours or the cognitions) and does not attempt to address the underlying issues that cause the problem. The goal is simply to stop the negative cycle by intervening to change cognition or behaviour. The client and the therapist work together to develop the goals of the therapy, the particular ways that the goals will be reached, and the timeline for reaching them. The procedures are problem-solving and action-oriented, and the client is forced to take responsibility for their own treatment. The client is assigned tasks to complete that will help improve the disorder and takes an active part in the therapy. The treatment usually lasts between 10 and 20 sessions. Depending on the particular disorder, some CBT treatments may be primarily behavioural in orientation, focusing on the principles of classical, operant, and observational learning, whereas other treatments are more cognitive, focused on changing negative thoughts related to the disorder. However, almost all CBT treatments use a combination of behavioural and cognitive approaches.
Behavioural aspects of CBT
In some cases, the primary changes that need to be made are behavioural. Behaviour therapy is psychological treatment that is based on principles of learning. The most direct approach is through operant conditioning using reward or punishment. Reinforcement may be used to teach new skills to people, such as with those with autism or schizophrenia (Granholm et al., 2008; Herbert et al., 2005; Scattone, 2007). If the patient has trouble dressing or grooming, then reinforcement techniques, such as providing tokens that can be exchanged for snacks, are used to reinforce appropriate behaviours, such as putting on one’s clothes in the morning or taking a shower at night. If the patient has trouble interacting with others, reinforcement will be used to teach the client how to respond more appropriately in public, for instance, by maintaining eye contact, smiling when appropriate, and modulating tone of voice.
As the patient practises the different techniques, the appropriate behaviours are shaped through reinforcement to allow the client to manage more complex social situations. In some cases, observational learning may also be used; the client may be asked to observe the behaviour of others who are more socially skilled to acquire appropriate behaviours. People who learn to improve their interpersonal skills through skills training may be more accepted by others, and this social support may have substantial positive effects on their emotions.
When the disorder is anxiety or phobia, then the goal of the CBT is to reduce the negative affective responses to the feared stimulus. Exposure therapy is a behavioural therapy based on the classical conditioning principle of extinction, in which people are confronted with a feared stimulus with the goal of decreasing their negative emotional responses to it (Wolpe, 1973). Exposure treatment can be carried out in real situations or through imagination, and it is used in the treatment of panic disorder, agoraphobia, social phobia, OCD, and post-traumatic stress disorder (PTSD).
In flooding, a client is exposed to the source of their fear all at once. An agoraphobic might be taken to a crowded shopping mall, or someone with an extreme fear of heights might be taken to the top of a tall building. The assumption is that the fear will subside as the client habituates to the situation while receiving emotional support from the therapist during the stressful experience. An advantage of the flooding technique is that it is quick and often effective, but a disadvantage is that the patient may relapse after a short period of time.
More frequently, the exposure is done more gradually. Systematic desensitization is a behavioural treatment that combines imagining or experiencing the feared object or situation with relaxation exercises (Wolpe, 1973). The client and the therapist work together to prepare a hierarchy of fears, starting with the least frightening and moving to the most frightening scenario surrounding the object. Refer to the table below for an example. The patient then confronts the fears in a systematic manner, sometimes using their imagination but usually, when possible, in real life.
| Behaviour | Fear Rating |
|---|---|
| Think about a spider. | 10 |
| Look at a photo of a spider. | 25 |
| Look at a real spider in a closed box. | 50 |
| Hold the box with the spider. | 60 |
| Let a spider crawl on your desk. | 70 |
| Let a spider crawl on your shoe. | 80 |
| Let a spider crawl on your pants leg. | 90 |
| Let a spider crawl on your sleeve. | 95 |
| Let a spider crawl on your bare arm. | 100 |
Desensitization techniques use the principle of counter-conditioning, in which a second incompatible response (e.g., relaxation through deep breathing) is conditioned to an already conditioned response (e.g., the fear response). The continued pairing of the relaxation responses with the feared stimulus as the patient works up the hierarchy gradually leads the fear response to be extinguished and the relaxation response to take its place.
Behaviour therapy works best when people directly experience the feared object. Fears of spiders are more directly habituated when the patient interacts with a real spider, and fears of flying are best extinguished when the patient gets on a real plane. However, it is often difficult and expensive to create these experiences for the patient. Recent advances in virtual reality have allowed clinicians to provide CBT in what seem like real situations to the patient. In virtual reality CBT, the therapist uses computer-generated, three-dimensional, lifelike images of the feared stimulus in a systematic desensitization program. Specially designed computer equipment, often with a head-mount display, is used to create a simulated environment. A common use is in helping patients who are experiencing PTSD return to the scene of the trauma and learn how to cope with the stress it invokes.
Some of the advantages of the virtual reality treatment approach are that it is economical, the treatment session can be held in the therapist’s office with no loss of time or confidentiality, the session can easily be terminated as soon as a patient feels uncomfortable, and many patients who have resisted live exposure to the object of their fears are willing to try the new virtual reality option first.
Aversion therapy is a type of behaviour therapy in which positive punishment is used to reduce the frequency of an undesirable behaviour. An unpleasant stimulus is intentionally paired with a harmful or socially unacceptable behaviour until the behaviour becomes associated with unpleasant sensations and is hopefully reduced. For example, a child who wets their bed may be required to sleep on a pad that sounds an alarm when it senses moisture. Over time, the positive punishment produced by the alarm reduces the bedwetting behaviour (Houts, Berman, & Abramson, 1994). Aversion therapy is also used to stop other specific behaviours, such as nail biting (Allen, 1996).
Alcoholism has long been treated with aversion therapy (Baker & Cannon, 1988). In a standard approach, patients are treated at a hospital where they are administered a drug, antabuse, that makes them nauseous if they consume any alcohol. The technique works very well if the user keeps taking the drug (Krampe et al., 2006), but unless it is combined with other approaches, the patients are likely to relapse after they stop taking the drug.
Cognitive aspects of CBT
While behavioural approaches focus on the actions of the patient, cognitive therapy is a psychological treatment that helps clients identify incorrect or distorted beliefs that are contributing to disorder. In cognitive therapy, the therapist helps the patient develop new, healthier ways of thinking about themselves and about the others around them. The idea of cognitive therapy is that changing thoughts will change emotions and that the new emotions will then influence behaviour.
The goal of cognitive therapy is not necessarily to get people to think more positively, but rather to think more accurately. For instance, a person who thinks “no one cares about me” is likely to feel rejected, isolated, and lonely. If the therapist can remind the person that they have a parent, partner, or child who does care about them, more positive feelings will likely follow. Similarly, changing beliefs from “I have to be perfect” to “no one is always perfect; I’m doing pretty good,” from “I am a terrible student” to “I am doing well in some of my courses,” or from “they did that on purpose to hurt me” to “maybe they didn’t realize how important it was to me” may all be helpful.
The psychiatrist Aaron Beck and the psychologist Albert Ellis (1913–2007) together provided the basic principles of cognitive therapy. Ellis (2004) called this approach rational emotive behaviour therapy (REBT) or rational emotive therapy (RET) and focused on pointing out the flaws in the patient’s thinking. Ellis noticed that people experiencing strong negative emotions tend to personalize and overgeneralize their beliefs, leading to an inability to see situations accurately (Leahy, 2003). In REBT, the therapist’s goal is to challenge these irrational thought patterns, helping the patient replace the irrational thoughts with more rational ones, leading to the development of more appropriate emotional reactions and behaviours.
Aaron Beck’s cognitive therapy was based on his observation that people who were depressed generally had a large number of highly accessible negative thoughts that influenced their thinking (J. S. Beck, 1995; A. T. Beck, Freeman, & Davis, 2004). His goal was to develop a short-term therapy for depression that would modify these unproductive thoughts. Beck’s approach challenges the client to test their beliefs against concrete evidence. If a client claims that “everybody at work is out to get me,” the therapist might ask the client to provide instances to corroborate the claim. At the same time, the therapist might point out contrary evidence, such as the fact that a certain coworker is actually a loyal friend or that the patient’s boss had recently praised them.
Advantages and disadvantages of CBT
CBT interventions tend to be relatively brief, making them cost-effective for the average consumer. In addition, CBT is an intuitive treatment that makes logical sense to patients. It can also be adapted to suit the needs of many different populations. One disadvantage, however, is that CBT does involve significant effort on the patient’s part because the patient is an active participant in treatment. Therapists often assign “homework” (e.g., worksheets for recording one’s thoughts and behaviours) between sessions to maintain the cognitive and behavioural habits the patient is working on. The greatest strength of CBT is the abundance of empirical support for its effectiveness. Studies have consistently found CBT to be equally or more effective than other forms of treatment, including medication and other therapies (Butler, Chapman, Forman, & Beck, 2006; Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012). For this reason, CBT is considered a first-line treatment for many mental disorders.
Acceptance and mindfulness-based approaches
Unlike the preceding therapies, which were developed in the 20th century, this next one was born out of age-old Buddhist and yoga practices. Mindfulness, or a process that tries to cultivate a nonjudgmental, yet attentive, mental state, is a therapy that focuses on one’s awareness of bodily sensations, thoughts, and the outside environment. Whereas other therapies work to modify or eliminate these sensations and thoughts, mindfulness focuses on nonjudgmentally accepting them (Kabat-Zinn, 2003; Baer, 2003). For example, whereas CBT may actively confront and work to change a maladaptive thought, mindfulness therapy works to acknowledge and accept the thought, understanding that the thought is spontaneous and not what the person truly believes. There are two important components of mindfulness: self-regulation of attention and orientation toward the present moment (Bishop et al., 2004). Mindfulness is thought to improve mental health because it draws attention away from past and future stressors, encourages acceptance of troubling thoughts and feelings, and promotes physical relaxation.
Techniques in mindfulness-based therapy
Psychologists have adapted the practice of mindfulness as a form of psychotherapy, generally called mindfulness-based therapy (MBT). Several types of MBT have become popular in recent years, including mindfulness-based stress reduction (Kabat-Zinn, 1982) and mindfulness-based cognitive therapy (Segal, Williams, & Teasdale, 2002).
Mindfulness-based stress reduction (MBSR) uses meditation, yoga, and attention to physical experiences to reduce stress (see Figure 16.4). The hope is that reducing a person’s overall stress will allow that person to more objectively evaluate their thoughts. In mindfulness-based cognitive therapy (MBCT), rather than reducing one’s general stress to address a specific problem, attention is focused on one’s thoughts and their associated emotions. For example, MBCT helps prevent relapses in depression by encouraging patients to evaluate their own thoughts objectively and without value judgment (Baer, 2003). Although cognitive behavioural therapy (CBT) may seem similar to this, it focuses on “pushing out” the maladaptive thought, whereas mindfulness-based cognitive therapy focuses on “not getting caught up” in it. The treatments used in MBCT have been used to address a wide range of illnesses, including depression, anxiety, chronic pain, coronary artery disease, and fibromyalgia (Hofmann, Sawyer, Witt & Oh, 2010).

Mindfulness and acceptance — in addition to being therapies in their own right — have also been used as “tools” in other cognitive-behavioural therapies, particularly in dialectical behaviour therapy (e.g., Linehan, Amstrong, Suarez, Allmon, & Heard, 1991). Dialectical behaviour therapy (DBT), often used in the treatment of borderline personality disorder, focuses on skills training. That is, it often employs mindfulness and cognitive behavioural therapy practices, but it also works to teach its patients “skills” they can use to correct maladaptive tendencies. For example, one skill DBT teaches patients is called distress tolerance — that is, ways to cope with maladaptive thoughts and emotions in the moment. For example, people who feel an urge to cut themselves may be taught to snap their arm with a rubber band instead. The primary difference between DBT and CBT is that DBT employs techniques that address the symptoms of the problem (e.g., cutting oneself) rather than the problem itself (e.g., understanding the psychological motivation to cut oneself). CBT does not teach such skills training because of the concern that the skills — even though they may help in the short-term — may be harmful in the long-term, by maintaining maladaptive thoughts and behaviours.
DBT is founded on the perspective of a dialectical worldview. That is, rather than thinking of the world as “black and white,” or “only good and only bad,” it focuses on accepting that some things can have characteristics of both “good” and “bad.” So, in a case involving maladaptive thoughts, instead of teaching that a thought is entirely bad, DBT tries to help patients be less judgmental of their thoughts, as with mindfulness-based therapy, and encourages change through therapeutic progress, using cognitive-behavioural techniques as well as mindfulness exercises.
Another form of treatment that also uses mindfulness techniques is acceptance and commitment therapy (Hayes, Strosahl, & Wilson, 1999). In acceptance and commitment therapy (ACT), patients are taught to observe their thoughts from a detached perspective (Hayes et al., 1999). ACT encourages patients not to attempt to change or avoid thoughts and emotions they observe in themselves, but instead to recognize which are beneficial and which are harmful. However, the differences among ACT, CBT, and other mindfulness-based treatments are a topic of controversy in the current literature.
Advantages and disadvantages of mindfulness-based therapy
Two key advantages of mindfulness-based therapies are their acceptability and accessibility to patients. Because yoga and meditation are already widely known in popular culture, consumers of mental healthcare are often interested in trying related psychological therapies. Currently, psychologists have not come to a consensus on the efficacy of MBT, though growing evidence supports its effectiveness for treating mood and anxiety disorders. For example, one review of MBT studies for anxiety and depression found that mindfulness-based interventions generally led to moderate symptom improvement (Hofmann et al., 2010).
Emerging treatment strategies
With growth in research and technology, psychologists have been able to develop new treatment strategies in recent years. Often, these approaches focus on enhancing existing treatments, such as cognitive-behavioural therapies, through the use of technological advances. For example, internet- and mobile-delivered therapies make psychological treatments more available, through smartphones and online access. Clinician-supervised online CBT modules allow patients to access treatment from home on their own schedule — an opportunity particularly important for patients with less geographic or socioeconomic access to traditional treatments. Furthermore, smartphones help extend therapy to patients’ daily lives, allowing for symptom tracking, homework reminders, and more frequent therapist contact.

Another benefit of technology is cognitive bias modification. Here, patients are given exercises, often through the use of video games, aimed at changing their problematic thought processes. For example, researchers might use a mobile app to train alcohol abusers to avoid stimuli related to alcohol. One version of this game flashes four pictures on the screen — three alcohol cues (e.g., a can of beer or the front of a bar) and one health-related image (e.g., someone drinking water). The goal is for the patient to tap the healthy picture as fast as they can. Games like these aim to target patients’ automatic, subconscious thoughts that may be difficult to direct through conscious effort. That is, by repeatedly tapping the healthy image, the patient learns to “ignore” the alcohol cues, so when those cues are encountered in the environment, they will be less likely to trigger the urge to drink. Approaches like these are promising because of their accessibility; however, they require further research to establish their effectiveness.
Yet another emerging treatment employs CBT-enhancing pharmaceutical agents. These are drugs used to improve the effects of therapeutic interventions. Based on research from animal experiments, researchers have found that certain drugs influence the biological processes known to be involved in learning. Thus, if people take these drugs while going through psychotherapy, they are better able to “learn” the techniques for improvement. For example, the antibiotic d-cycloserine improves treatment for anxiety disorders by facilitating the learning processes that occur during exposure therapy. Ongoing research in this exciting area may prove to be quite fruitful.
Pharmacological treatments
Up until this point, all the therapies we have discussed have been talk-based or meditative practices. However, psychiatric medications are also frequently used to treat mental disorders, including schizophrenia, bipolar disorder, depression, and anxiety disorders. Psychiatric drugs are commonly used, in part, because they can be prescribed by general medical practitioners, whereas only trained psychologists are qualified to deliver effective psychotherapy. While drugs and CBT therapies tend to be almost equally effective, choosing the best intervention depends on the disorder and individual being treated, as well as factors such as treatment availability and comorbidity (i.e., having multiple mental or physical disorders at once). Although many new drugs have been introduced in recent decades, there is still much we do not understand about their mechanism in the brain. Further research is needed to refine our understanding of both pharmacological and behavioural treatments before we can make firm claims about their effectiveness.
Combination (eclectic) approaches to therapy
We have considered the different approaches to psychotherapy under the assumption that a therapist will use only one approach with a given patient, but this is not necessarily the case. The most commonly practised approach to therapy is an eclectic therapy, an approach to treatment in which the therapist uses whichever techniques seem most useful and relevant for a given patient. For bipolar disorder, for instance, the therapist may use both psychological skills training to help the patient cope with the severe highs and lows, but they are likely to also suggest that the patient consider drug therapies (Newman, Leahy, Beck, Reilly-Harrington, & Gyulai, 2002). Treatment for major depressive disorder usually involves antidepressant drugs as well as CBT to help the patient deal with particular problems (McBride, Farvolden, & Swallow, 2007).
Source: Adapted from Boettcher, Hofmann, and Wu (2020).
Key Takeaways
- Care providers with a variety of training, education, and experience provide help for mental disorders and psychological distress.
- Psychoanalysis is based on the principles of Freudian and neo-Freudian personality theories. The goal is to explore the unconscious dynamics of personality.
- Humanist therapy, derived from the personality theory of Carl Rogers, is based on the idea that people experience psychological problems when they are burdened by limits and expectations placed on them by themselves and others. Its focus is on helping people reach their life goals.
- Behaviour therapy applies the principles of classical and operant conditioning, as well as observational learning, to the elimination of maladaptive behaviours and their replacement with more adaptive responses.
- Albert Ellis and Aaron Beck developed cognitive-based therapies to help clients stop negative thoughts and replace them with more objective thoughts.
- Mindfulness approaches to therapy emphasize self-regulation of attention and orientation toward the present moment.
- Eclectic therapy is the most common approach to treatment. In eclectic therapy, the therapist uses whatever treatment approaches seem most likely to be effective for the client.
Exercises and Critical Thinking
- Imagine that your friend has been feeling depressed for several months but refuses to consider therapy as an option. What might you tell them that might help them feel more comfortable about seeking treatment?
- Imagine that you have developed a debilitating fear of bees after recently being attacked by a swarm of them. What type of therapy do you think would be best for your disorder?
- Imagine that your friend has a serious drug abuse problem. Based on what you’ve learned in this section, what treatment options would you explore in your attempt to provide them with the best help available? Which combination of therapies might work best?
- Psychoanalytic theory is no longer the dominant therapeutic approach because it lacks empirical support. Yet, many consumers continue to seek psychoanalytic or psychodynamic treatments. Do you think psychoanalysis still has a place in mental health treatment? If so, why?
- What might be some advantages and disadvantages of using technology in psychological treatment? What will psychotherapy look like 100 years from now?
Image Attributions
Figure 16.2. Used under a CC BY-NC-SA 4.0 license.
Figure 16.3. Carl Ransom Rogers by Didius is used under a CC BY 2.5 license.
Figure 16.4. Meditating in Union Station by Wayne MacPhail is used under a CC BY-NC-SA 2.0 license.
Figure 16.5. Used under a CC BY-NC-SA 4.0 license.
References
Allen, K. W. (1996). Chronic nailbiting: A controlled comparison of competing response and mild aversion treatments. Behaviour Research and Therapy, 34, 269–272.
Baer, R. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143.
Baker, T. B., & Cannon, D. S. (1988). Assessment and treatment of addictive disorders. New York, NY: Praeger.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders. New York, NY: New American Library.
Beck, A. T., Freeman, A., & Davis, D. D. (2004). Cognitive therapy of personality disorders (2nd ed.). New York, NY: Guilford Press.
Beck, J. S. (1995). Cognitive therapy: Basics and beyond. New York, NY: Guilford Press.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., . . . Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241.
Boettcher, H., Hofmann, S. G., & Wu, Q. J. (2020). Therapeutic orientations. In R. Biswas-Diener & E. Diener (Eds.), Noba textbook series: Psychology. Champaign, IL: DEF. Retrieved from http://noba.to/fjtnpwsk
Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26, 17–31.
Canadian Mental Health Association. (2013). Mental health. Retrieved from http://www.cmha.ca/mental-health
Cuijpers, P., Driessen, E., Hollon, S.D., van Oppen, P., Barth, J., & Andersson, G. (2012). The efficacy of non-directive supportive therapy for adult depression: A meta-analysis. Clinical Psychology Review, 32, 280–291.
Driessen, E., Cuijpers, P., de Maat, S. C. M., Abbass, A. A., de Jonghe, F., & Dekker, J. J. M. (2010). The efficacy of short-term psychodynamic psychotherapy for depression: A meta-analysis. Clinical Psychology Review, 30, 25–36.
Ellis, A. (2004). Why rational emotive behavior therapy is the most comprehensive and effective form of behavior therapy. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 22, 85–92.
Freud, S. (1955). Beyond the pleasure principle. London, England: Hogarth Press. (Original work published 1920)
Freud, S. (1955). Studies on hysteria. London, England: Hogarth Press. (Original work published 1895)
Freud, S. (1955). The interpretation of dreams. London, England: Hogarth Press. (Original work published 1900)
Friedli, K., King, M. B., Lloyd, M., & Horder, J. (1997). Randomized controlled assessment of non-directive psychotherapy versus routine general-practitioner care. The Lancet Psychiatry, 350, 1662–1665.
Granholm, E., McQuaid, J. R., Link, P. C., Fish, S., Patterson, T., & Jeste, D. V. (2008). Neuropsychological predictors of functional outcome in cognitive behavioral social skills training for older people with schizophrenia. Schizophrenia Research, 100, 133–143.
Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and commitment therapy. New York, NY: Guilford Press.
Herbert, J. D., Gaudini, B. A., Rheingold, A. A., Myers, V. H., Dalrymple, K., & Nolan, E. M. (2005). Social skills training augments the effectiveness of cognitive behavioral group therapy for social anxiety disorder. Behavior Therapy, 36, 125–138.
Hofmann, S. G., Asnaani, A., Vonk, J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36, 427–440.
Hofmann, S. G., Sawyer, A. T., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183
Houts, A. C., Berman, J. S., & Abramson, H. (1994). Effectiveness of psychological and pharmacological treatments for nocturnal enuresis. Journal of Consulting and Clinical Psychology, 62(4), 737–745.
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156.
Krampe, H., Stawicki, S., Wagner, T., Bartels, C., Aust, C., Rüther, E., . . . Ehrenreich, H. (2006). Follow-up of 180 alcoholic patients for up to 7 years after outpatient treatment: Impact of alcohol deterrents on outcome. Alcoholism: Clinical and Experimental Research, 30(1), 86–95.
Leahy, R. L. (2003). Cognitive therapy techniques: A practitioner’s guide. New York, NY: Guilford Press.
Leichsenring, F., & Rabung, S. (2008). Effectiveness of long-term psychodynamic psychotherapy: A meta-analysis. Journal of the American Medical Association, 300, 1551–1565.
Linehan, M. M., Amstrong, H.-E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically suicidal borderline patients. Archives of General Psychiatry, 48, 1060–1064.
McBride, C., Farvolden, P., & Swallow, S. R. (2007). Major depressive disorder and cognitive schemas. In L. P. Riso, P. L. du Toit, D. J. Stein, & J. E. Young (Eds.), Cognitive schemas and core beliefs in psychological problems: A scientist-practitioner guide (pp. 11–39). Washington, DC: American Psychological Association.
National Inquiry into Missing and Murdered Indigenous Women and Girls. (2019). Aftercare services. Retrieved from https://www.mmiwg-ffada.ca/aftercare-services
Newman, C. F., Leahy, R. L., Beck, A. T., Reilly-Harrington, N. A., & Gyulai, L. (2002). Clinical management of depression, hopelessness, and suicidality in patients with bipolar disorder. In C. F. Newman, R. L. Leahy, A. T. Beck, N. A. Reilly-Harrington, & L. Gyulai (Eds.), Bipolar disorder: A cognitive therapy approach (pp. 79–100). Washington, DC: American Psychological Association.
Prochaska, J. O., & Norcross, J. C. (2007). Systems of psychotherapy: A transtheoretical analysis (6th ed.). Pacific Grove, CA: Brooks/Cole.
Rogers, C. (1980). A way of being. New York, NY: Houghton Mifflin.
Scattone, D. (2007). Social skills interventions for children with autism. Psychology in the Schools, 44(7), 717–726.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: Guilford Press.
Wolpe, J. (1973). The practice of behavior therapy. New York, NY: Pergamon.

