15.1 Psychological Disorder: The Challenges of Definition
Learning Objectives
- Define psychological disorder, and summarize the general causes of disorder.
- Explain why it is so difficult to define disorder.
- Describe the stigma of psychological disorders and their impact on those who suffer from them.
In 2012, approximately 2.8 million people, or 10.1% of Canadians aged 15 and older, reported symptoms consistent with at least one of six mental or substance use disorders in the past 12 months (Pearson, Janz, & Ali, 2013). At least a half billion people are affected worldwide. The six disorders measured by the Canadian Mental Health Survey were major depressive episode, bipolar disorder, generalized anxiety disorder, and abuse of or dependence on alcohol, cannabis, or other drugs. The impact of mental illness is particularly strong on people who are poorer, of lower socioeconomic class, and from disadvantaged ethnic groups.
People with psychological disorders are also stigmatized by the people around them, resulting in feelings of shame and embarrassment as well as prejudice and discrimination against them. Thus, the understanding and treatment of psychological disorder has broad implications for the everyday life of many people. The table below shows the prevalence, the frequency of occurrence of a given condition in a population at a given time, of some of the major psychological disorders in Canada.
| Disorder | Lifetime | 12-Month | |
|---|---|---|---|
| Substance use disorder | Alcohol abuse or dependence | 18.1% | 3.2% |
| Cannabis abuse or dependence | 6.8% | 1.3% | |
| Other drug abuse or dependence | 4% | 0.7% | |
| Total substance use disorders | 21.6% | 4.4% | |
| Mood disorder | Major depressive episode | 11.3% | 4.7% |
| Bipolar disorder | 2.6% | 1.5% | |
| Generalized anxiety disorder | 8.7% | 2.6% | |
| Total mood disorders | 12.6% | 5.4% | |
| Total mental or substance disorders | 33.1% | 10.1% | |
| Data source: Pearson, Janz, and Ali, 2013. | |||
In this chapter, our focus is on the disorders themselves. We will review the major psychological disorders and consider their causes and their impact on the people who suffer from them. Then, in Chapter 16. Treating Psychological Disorders, we will turn to consider the treatment of these disorders through psychotherapy and drug therapy.
Defining disorder
A psychological disorder is an ongoing dysfunctional pattern of thought, emotion, and behaviour that causes significant distress and that is considered deviant in that person’s culture or society (Butcher, Mineka, & Hooley, 2007). Psychological disorders have much in common with other medical disorders. They are out of the patient’s control, they may in some cases be treated by drugs, and their treatment is often covered by medical insurance. Like medical problems, psychological disorders have both biological (i.e., nature) as well as environmental (i.e., nurture) influences. These causal influences are reflected in the bio-psycho-social model of illness (Engel, 1977).
The bio-psycho-social model of illness is a way of understanding disorder that assumes that disorder is caused by biological, psychological, and social factors (see Figure 15.1). The biological component of the bio-psycho-social model refers to the influences on disorder that come from the functioning of the individual’s body; particularly important are genetic characteristics, which may make some people more vulnerable to a disorder than others, and the influence of neurotransmitters. The psychological component of the bio-psycho-social model refers to the influences that come from the individual, such as patterns of negative thinking and stress responses. The social component of the bio-psycho-social model refers to the influences on disorder due to social and cultural factors, such as socioeconomic status, homelessness, abuse, and discrimination.
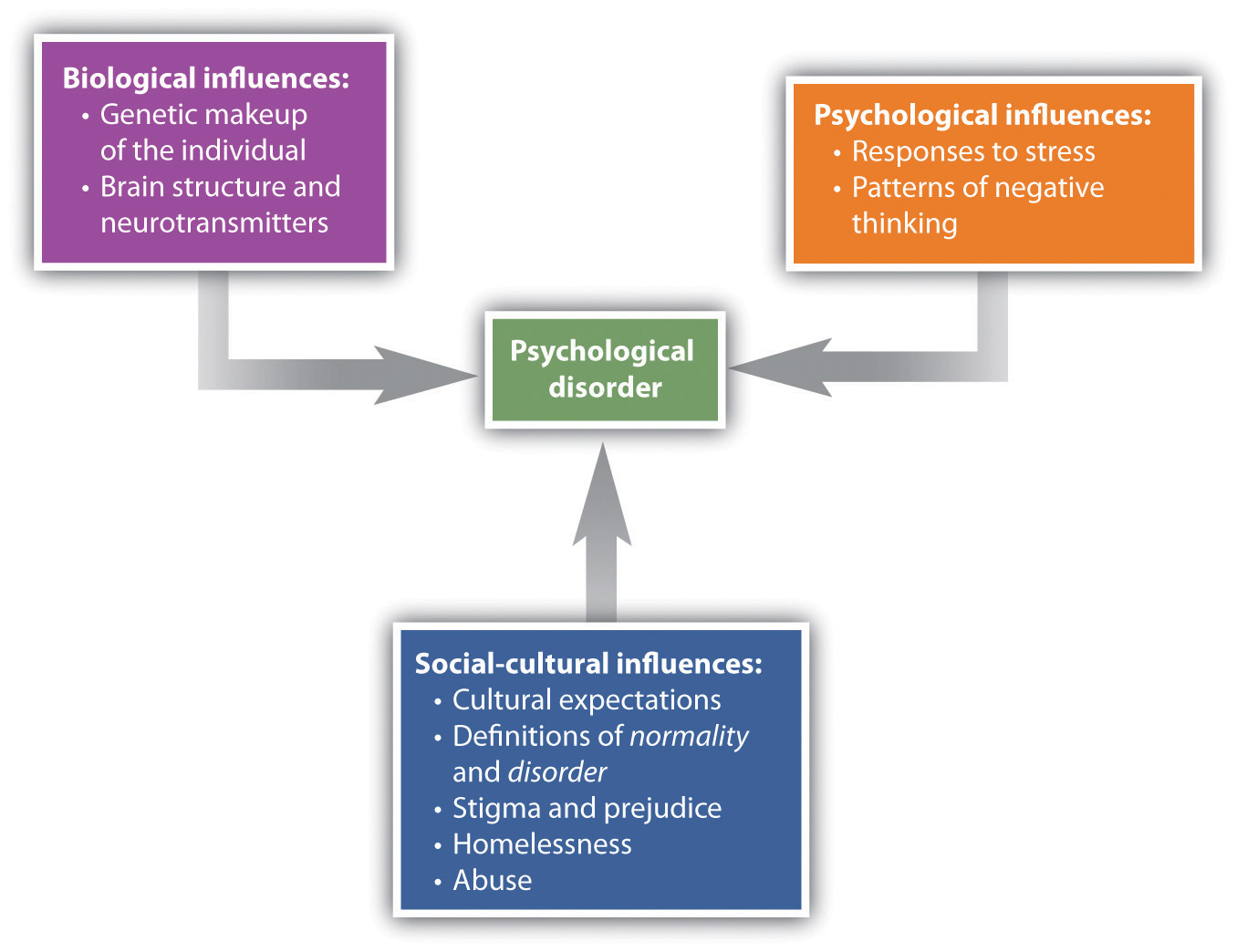
To consider one example, the psychological disorder of schizophrenia has a biological cause because it is known that there are patterns of genes that make a person vulnerable to the disorder (Gejman, Sanders, & Duan, 2010). However, whether or not the person with a biological vulnerability experiences the disorder depends in large part on psychological factors, such as how the individual responds to the stress they experience, as well as social factors, such as whether or not the person is exposed to stressful environments in adolescence and whether or not the person has support from people who care about them (Sawa & Snyder, 2002; Walker, Kestler, Bollini, & Hochman, 2004). Similarly, mood and anxiety disorders are caused in part by genetic factors like hormones and neurotransmitters, in part by the individual’s particular thought patterns, and in part by the ways that other people in the social environment treat the person with the disorder. We will use the bio-psycho-social model as a framework for considering the causes and treatments of disorder.
Although they share many characteristics with them, psychological disorders are nevertheless different from medical conditions in important ways. For one, diagnosis of psychological disorders can be more difficult. Although a medical doctor can see cancer in the lungs using an MRI scan or see blocked arteries in the heart using cardiac catheterization, there is no corresponding test for psychological disorders. Current research is beginning to provide more evidence about the role of brain structures in psychological disorders, but for now, the brains of people with severe mental disturbances often look identical to those of people without such disturbances.
Because there are no clear biological diagnoses, psychological disorders are instead diagnosed on the basis of clinical observations of the behaviours that the individual engages in. These observations find that emotional states and behaviours operate on a continuum, ranging from more normal and accepted to more deviant, abnormal, and unaccepted. The behaviours that are associated with disorder are in many cases the same behaviours that we engage in during our normal everyday life. Washing one’s hands is a normal and healthy activity, but it can be overdone by those with an obsessive-compulsive disorder (OCD). Similarly, it is not unusual to worry about and try to improve one’s body image; for example, a dancer may need to be thin for their career, but when does their dieting turn into a psychological disorder? Psychologists believe this happens when the behaviour becomes distressing and dysfunctional to the person.
Whether a given behaviour is considered a psychological disorder is determined not only by whether a behaviour is unusual (e.g., whether it is mild anxiety versus extreme anxiety), but also by whether a behaviour is maladaptive — that is, the extent to which it causes distress (e.g., pain and suffering to the person or those around them) and dysfunction (e.g., impairment in one or more important areas of functioning) to the individual (American Psychiatric Association, 2013). An intense fear of spiders, for example, would not be considered a psychological disorder unless it has a significant negative impact on the sufferer’s life, such as causing them to be unable to step outside the house. The focus on distress and dysfunction means that behaviours that are simply unusual or statistically rare — such as some political, religious, or sexual practices — are not classified as disorders.
Put your psychology hat on for a moment, and consider the behaviours of the people listed in the table below. For each, indicate whether you think the behaviour is or is not a psychological disorder. If you’re not sure, what other information would you need to know to be more certain of your diagnosis?
| Yes | No | Need More Information | Description |
|---|---|---|---|
| Jackie frequently talks to herself while she is working out her math homework. Her roommate sometimes hears her and wonders if she is okay. | |||
| Charlie believes that the noises made by cars and planes going by outside his house have secret meanings. He is convinced that he was involved in the start of a nuclear war and that the only way for him to survive is to find the answer to a difficult riddle. | |||
| Harriet gets very depressed during the winter months when the light is low. She sometimes stays in her pajamas for the whole weekend, eating chocolate and watching TV. | |||
| Frank seems to be afraid of a lot of things. He worries about driving on the highway and about severe weather that may come through his neighbourhood, but mostly, he fears mice and checks under his bed frequently to see if any are present. | |||
| A worshiper speaking in “tongues” at an Evangelical church views himself as filled with the Holy Spirit and is considered blessed with the gift to speak the “language of angels.” |
A trained clinical psychologist would have checked off “need more information” for each of the examples in the table above, because although the behaviours may seem unusual, there is no clear evidence that they are distressing or dysfunctional for the person. Talking to ourselves out loud is unusual and can be a symptom of schizophrenia, but just because we do it once in a while does not mean that there is anything wrong with us. It is natural to be depressed, particularly in the long winter nights, but how severe should this depression be, and how long should it last? If the negative feelings last for an extended time and begin to lead the person to miss work or classes, then they may become symptoms of a mood disorder. It is normal to worry about things, but when does worry turn into a debilitating anxiety disorder? What about thoughts that seem to be irrational, such as being able to speak the language of angels? Are they indicators of a severe psychological disorder, or are they part of a normal religious experience? Again, the answer lies in the extent to which they are, or are not, interfering with the individual’s functioning in society.
Psychological disorder is most commonly diagnosed using the Diagnostic and Statistical Manual of Mental Disorders (DSM). It is periodically updated and is currently in the 5th revision. We will examine the use of the DSM more closely in the next section.
Another difficulty in diagnosing psychological disorders is that they frequently occur together. For instance, people diagnosed with anxiety disorders also often have mood disorders (Hunt, Slade, & Andrews, 2004), and people diagnosed with one personality disorder frequently suffer from other personality disorders as well. Comorbidity occurs when people who suffer from one disorder also suffer at the same time from other disorders. Because many psychological disorders are comorbid, most severe mental disorders are concentrated in a small group of people, about 6% of the population, who have more than three of them (Kessler, Chiu, Demler, & Walters, 2005).
Key Takeaways
- More psychologists are involved in the diagnosis and treatment of psychological disorder than in any other endeavour, and those tasks are probably the most important psychologists face.
- The impact on people with a psychological disorder comes both from the disease itself and from the stigma associated with disorder.
- A psychological disorder is an ongoing dysfunctional pattern of thought, emotion, and behaviour that causes significant distress and that is considered deviant in that person’s culture or society.
- According to the bio-psycho-social model, psychological disorders have biological, psychological, and social causes.
- It is difficult to diagnose psychological disorders, although the DSM provides guidelines. The DSM is frequently revised, taking into consideration new knowledge as well as changes in cultural norms about disorder.
Exercises and Critical Thinking
- Do you or your friends hold stereotypes about the mentally ill? Can you think of or find clips from any films or other popular media that portray mental illness positively or negatively? Is it more or less acceptable to stereotype the mentally ill than to stereotype other social groups?
- Consider the diagnosis of attention-deficit/hyperactivity disorder (ADHD), autism, and Asperger’s disorder from the biological, personal, and social-cultural perspectives. Do you think that these disorders are overdiagnosed? How might clinicians determine if ADHD is dysfunctional or distressing to the individual?
Image Attributions
Figure 15.1. Used under a CC BY-NC-SA 4.0 license.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Butcher, J., Mineka, S., & Hooley, J. (2007). Abnormal psychology and modern life (13th ed.). Boston, MA: Allyn & Bacon.
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129–136.
Gejman, P., Sanders, A., & Duan, J. (2010). The role of genetics in the etiology of schizophrenia. Psychiatric Clinics of North America, 33(1), 35–66.
Hunt, C., Slade, T., & Andrews, G. (2004). Generalized anxiety disorder and major depressive disorder comorbidity in the National Survey of Mental Health and Well Being. Depression and Anxiety, 20, 23–31.
Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627.
Pearson, C., Janz, T., & Ali, J. (2013). Health at a glance: Mental and substance use disorders in Canada (Catalogue no. 82-624-X). Retrieved from http://www.statcan.gc.ca/pub/82-624-x/2013001/article/11855-eng.pdf
Sawa, A., & Snyder, S. (2002). Schizophrenia: Diverse approaches to a complex disease. Science, 296(5568), 692–695.
Walker, E., Kestler, L., Bollini, A., & Hochman, K. (2004). Schizophrenia: Etiology and course. Annual Review of Psychology, 55, 401–430.

