12.5 Promoting Wellness
Learning Objectives
- Describe basic terminology used in the field of health psychology.
- Explain theoretical models of health, as well as the role of psychological stress in the development of disease.
- Describe psychological factors that contribute to resilience and improved health.
- Defend the relevance and importance of psychology to the field of medicine.
What is health psychology?
Today, we face more chronic disease than ever before because we are living longer lives while also frequently behaving in unhealthy ways. One example of a chronic disease is coronary heart disease (CHD); it is the number one cause of death worldwide (World Health Organization, 2013). CHD develops slowly over time and typically appears midlife, but related heart problems can persist for years after the original diagnosis or cardiovascular event. In managing illnesses that persist over time — other examples might include cancer, diabetes, and long-term disability — many psychological factors will determine the progression of the ailment. For example, do patients seek help when appropriate? Do they follow doctor recommendations? Do they develop negative psychological symptoms due to lasting illness (e.g., depression)? It is also important that psychological factors can play a significant role in who develops these diseases, the prognosis, and the nature of the symptoms related to the illness. Health psychology is a relatively new, interdisciplinary field of study that focuses on these very issues, or more specifically, the role of psychology in maintaining health, as well as preventing and treating illness.

Consideration of how psychological and social factors influence health is especially important today because many of the leading causes of illness in developed countries are often attributed to psychological and behavioural factors. In the case of CHD, discussed above, psychosocial factors — such as excessive stress, smoking, unhealthy eating habits, and some personality traits — can also lead to increased risk of disease and worse health outcomes. That being said, many of these factors can be adjusted using psychological techniques. For example, clinical health psychologists can improve health practices like poor dietary choices and smoking, they can teach important stress reduction techniques, and they can help treat psychological disorders tied to poor health. Health psychology considers how the choices we make, the behaviours we engage in, and even the emotions that we feel, can play an important role in our overall health (Cohen & Herbert, 1996; Taylor, 2012).
Health psychology relies on the Biopsychosocial Model of Health. This model posits that biology, psychology, and social factors are just as important in the development of disease as biological causes (e.g., germs, viruses), which is consistent with the World Health Organization (1946) definition of health. This model replaces the older Biomedical Model of Health, which primarily considers the physical, or pathogenic, factors contributing to illness. Thanks to advances in medical technology, there is a growing understanding of the physiology underlying the mind–body connection, and in particular, the role that different feelings can have on our body’s function. Health psychology researchers working in the fields of psychosomatic medicine and psychoneuroimmunology, for example, are interested in understanding how psychological factors can “get under the skin” and influence our physiology in order to better understand how factors like stress can make us sick.
Stress and health
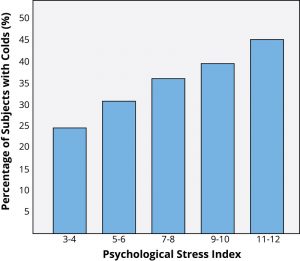
You probably know exactly what it’s like to feel stress, but what you may not know is that it can objectively influence your health. Answers to questions like “How stressed do you feel?” or “How overwhelmed do you feel?” can predict your likelihood of developing both minor illnesses as well as serious problems like future heart attack (Cohen, Janicki-Deverts, & Miller, 2007). To understand how health psychologists study these types of associations, we will describe one famous example of a stress and health study. Imagine that you are a research subject for a moment. After you check into a hotel room as part of the study, the researchers ask you to report your general levels of stress. Not very surprising so far; however, what happens next is that you receive droplets of coldvirus into your nose! The researchers intentionally try to make you sick by exposing you to an infectious illness. After they expose you to the virus, the researchers will then evaluate you for several days by asking you questions about your symptoms, monitoring how much mucus you are producing by weighing your used tissues, and taking body fluid samples — all to see if you are objectively ill with a cold. Now, the interesting thing is that not everyone who has drops of cold virus put in their nose develops the illness (see Figure 12.23). Studies like this one find that people who are less stressed and those who are more positive at the beginning of the study are at a decreased risk of developing a cold (Cohen, Tyrrell, & Smith, 1991; Cohen, Alper, Doyle, Treanor, & Turner, 2006).
Protecting our health
Health psychologists ask about the things that keep us protected from disease and alive longer. When considering this issue of resilience (Rutter, 1985), five factors are often studied in terms of their ability to protect, or sometimes harm, health. They are:
- Coping
- Control and Self-Efficacy
- Social Relationships
- Dispositions and Emotions
- Stress Management
Coping strategies
How individuals cope with the stressors they face can have a significant impact on health. Coping is often classified into two categories: problem-focused coping or emotion-focused coping (Carver, Scheier, & Weintraub, 1989). Problem-focused coping thought of as actively addressing the event that is causing stress in an effort to solve the issue at hand. For example, say you have an important exam coming up next week. A problem-focused strategy might be to spend additional time over the weekend studying to make sure you understand all of the material. Emotion-focused coping, on the other hand, regulates the emotions that come with stress. In the above examination example, this might mean watching a funny movie to take your mind off the anxiety you are feeling. In the short term, emotion-focused coping might reduce feelings of stress, but problem-focused coping seems to have the greatest impact on mental wellness (Billings & Moos, 1981; Herman-Stabl, Stemmler, & Petersen, 1995). That being said, when events are uncontrollable (e.g., the death of a loved one), emotion-focused coping directed at managing your feelings, at first, might be the better strategy. Therefore, it is always important to consider the match of the stressor to the coping strategy when evaluating its plausible benefits.
Control and self-efficacy
Another factor tied to better health outcomes and an improved ability to cope with stress is having the belief that you have control over a situation. For example, in one study where participants were forced to listen to unpleasant (i.e., stressful) noise, those who were led to believe that they had control over the noise performed much better on proofreading tasks afterwards (Glass & Singer, 1972). In other words, even though participants did not have actual control over the noise, the control belief aided them in completing the task. In similar studies, perceived control benefited immune system functioning (Sieber et al., 1992). Outside of the laboratory, studies have shown that older residents in assisted living facilities, which are notorious for low control, lived longer and showed better health outcomes when given control over something as simple as watering a plant or choosing when student volunteers came to visit (Rodin & Langer, 1977; Schulz & Hanusa, 1978). In addition, feeling in control of a threatening situation can actually change stress hormone levels (Dickerson & Kemeny, 2004). Believing that you have control over your own behaviours can also have a positive influence on important outcomes like smoking cessation, contraception use, and weight management (Wallston & Wallston, 1978). When individuals do not believe they have control, they do not try to change. Self-efficacy is closely related to control, in that people with high levels of this trait believe they can complete tasks and reach their goals. Just as feeling in control can reduce stress and improve health, higher self-efficacy can reduce stress and negative health behaviours, and it is associated with better health (O’Leary, 1985).

Social relationships
Research has shown that the impact of social isolation on our risk for disease and death is similar in magnitude to the risk associated with smoking regularly (Holt-Lunstad, Smith, & Layton, 2010; House, Landis, & Umberson, 1988). In fact, the importance of social relationships for our health is so significant that some scientists believe our body has developed a physiological system that encourages us to seek out our relationships, especially in times of stress (Taylor et al., 2000). Social integration is the concept used to describe the number of social roles that you have (Cohen & Wills, 1985), as well as the lack of isolation. For example, you might be a daughter, a basketball team member, a Humane Society volunteer, a coworker, and a student. Maintaining these different roles can improve your health via encouragement from those around you to maintain a healthy lifestyle. Those in your social network might also provide you with social support when you are under stress. This support might include emotional help (e.g., a hug when you need it), tangible help (e.g., lending you money), or advice. By helping to improve health behaviours and reduce stress, social relationships can have a powerful, protective impact on health and, in some cases, might even help people with serious illnesses stay alive longer (Spiegel, Kraemer, Bloom, & Gottheil, 1989).
Dispositions and emotions: What’s risky and what’s protective?
Negative dispositions and personality traits have been strongly tied to an array of health risks. One of the earliest negative trait-to-health connections was discovered in the 1950s by two cardiologists. They made the interesting discovery that there were common behavioural and psychological patterns among their heart patients that were not present in other patient samples. This pattern included being competitive, impatient, hostile, and time urgent. They labelled it Type A behaviour. Importantly, it was found to be associated with double the risk of heart disease as compared with Type B behaviour (Friedman & Rosenman, 1959). Since the 1950s, researchers have discovered that it is the hostility and competitiveness components of Type A behaviour that are especially harmful to heart health (Iribarren et al., 2000; Matthews, Glass, Rosenman, & Bortner, 1977; Miller, Smith, Turner, Guijarro, & Hallet, 1996). Hostile individuals are quick to get upset, and this angry arousal can damage the arteries of the heart. In addition, given their negative personality style, hostile people often lack a health-protective and supportive social network.
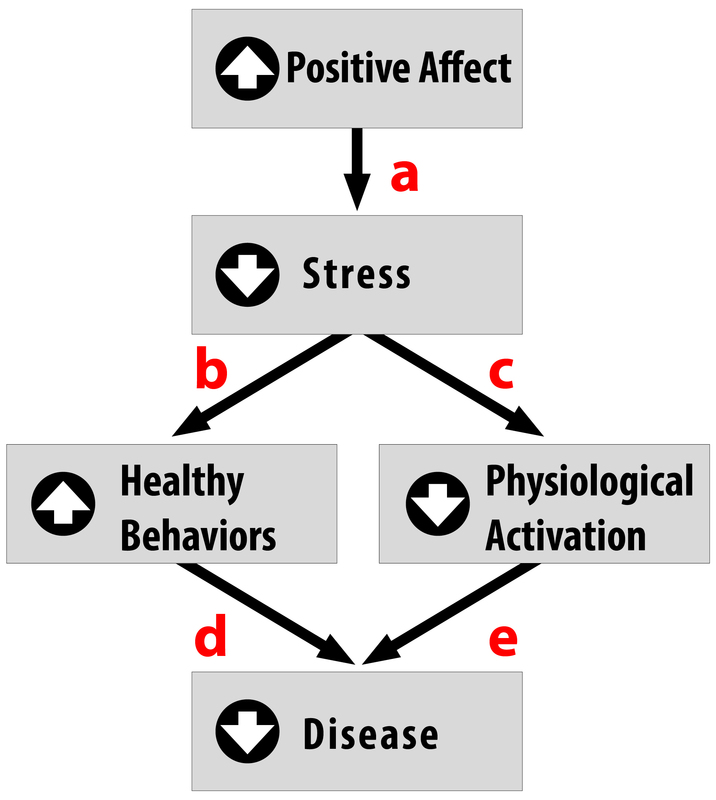
Positive traits and states, on the other hand, are often health-protective. For example, characteristics like positive emotions (e.g., feeling happy or excited) have been tied to a wide range of benefits such as increased longevity, a reduced likelihood of developing some illnesses, and better outcomes once you are diagnosed with certain diseases like heart disease and HIV (Pressman & Cohen, 2005). Across the world, even in the most poor and underdeveloped nations, positive emotions are consistently tied to better health (Pressman, Gallagher, & Lopez, 2013). Positive emotions can also serve as the “antidote” to stress (see Figure 12.25), protecting us against some of its damaging effects (Fredrickson, 2001; Pressman & Cohen, 2005). Similarly, looking on the bright side can also improve health. Optimism has been shown to improve coping, reduce stress, and predict better disease outcomes like recovering from a heart attack more rapidly (Kubzansky, Sparrow, Vokonas, & Kawachi, 2001; Nes & Segerstrom, 2006; Scheier & Carver, 1985; Segerstrom, Taylor, Kemeny, & Fahey, 1998).
Stress management
About 25% of Canadians report having stress, with 35-year-olds to 49-year-olds reporting the highest levels (Statistics Canada, 2019). Given that the sources of our stress are often difficult to change (e.g., personal finances or current job), a number of interventions have been designed to help reduce the aversive responses to duress. For example, relaxation activities and forms of meditation are techniques that allow individuals to reduce their stress via breathing exercises, muscle relaxation, and mental imagery. Physiological arousal from stress can also be reduced via biofeedback, which is a technique where the individual is shown bodily information that is not normally available to them (e.g., heart rate) and then taught strategies to alter this signal. This type of intervention has even shown promise in reducing heart and hypertension risk, as well as other serious conditions (e.g., Moravec, 2008; Patel, Marmot, & Terry, 1981), but reducing stress does not have to be complicated. For example, exercise is a great stress reduction activity (Salmon, 2001) that has plenty of health benefits.
The importance of good health practices
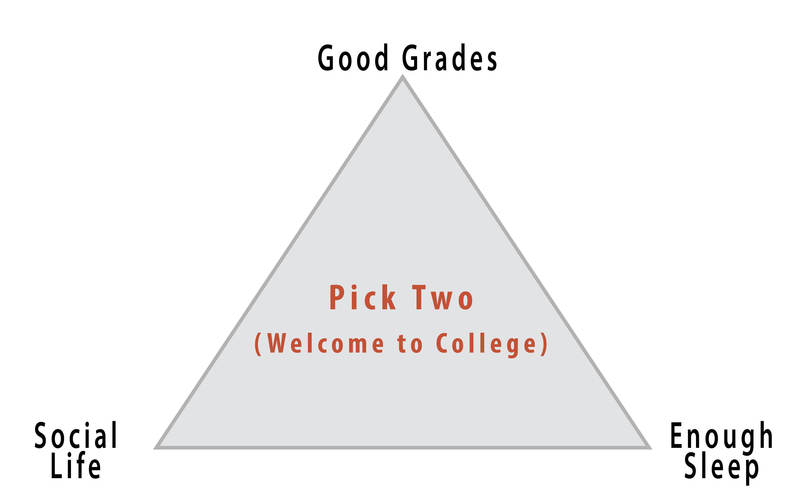
As a student, you probably strive to maintain good grades, to have an active social life, and to stay healthy (e.g., by getting enough sleep), but there is a popular joke about what it’s like to be in college: you can only pick two of these things (see Figure 12.26). The busy life of a college student doesn’t always allow you to maintain all three areas of your life, especially during test-taking periods. In one study, researchers found that students taking exams were more stressed and, thus, smoked more, drank more caffeine, had less physical activity, and had worse sleep habits (Oaten & Cheng, 2005), all of which could have detrimental effects on their health. Positive health practices are especially important in times of stress when your immune system is compromised due to high stress and the elevated frequency of exposure to the illnesses of your fellow students in lecture halls, cafeterias, and dorms.
Psychologists study both health behaviours and health habits. The former are behaviours that can improve or harm your health. Some examples include regular exercise, flossing, and wearing sunscreen, versus negative behaviours like drunk driving, pulling all-nighters, and smoking. These behaviours become habits when they are firmly established and performed automatically. For example, do you have to think about putting your seatbelt on, or do you do it automatically? Habits are often developed early in life thanks to parental encouragement or the influence of our peer group.
While these behaviours sound minor, studies have shown that those who engaged in more of these protective habits (e.g., getting 7–8 hours of sleep regularly, not smoking or drinking excessively, and exercising) had fewer illnesses, felt better, and were less likely to die over a 9–12-year follow-up period (Belloc & Breslow, 1972; Breslow & Enstrom, 1980). For college students, health behaviours can even influence academic performance. For example, poor sleep quality and quantity are related to weaker learning capacity and academic performance (Curcio, Ferrara, & De Gennaro, 2006). Due to the effects that health behaviours can have, much effort is put forward by psychologists to understand how to change unhealthy behaviours and to understand why individuals fail to act in healthy ways. Health promotion involves enabling individuals to improve health by focusing on behaviours that pose a risk for future illness, as well as spreading knowledge on existing risk factors. These might be genetic risks you are born with, or something you developed over time like obesity, which puts you at risk for type 2 diabetes and heart disease, among other illnesses.
Psychology and medicine
There are many psychological factors that influence medical treatment outcomes. For example, older individuals (Meara, White, & Cutler, 2004), women (Briscoe, 1987), and those from higher socioeconomic backgrounds (Adamson, Ben-Shlomo, Chaturvedi, & Donovan, 2003) are all more likely to seek medical care. On the other hand, some individuals who need care might avoid it due to financial obstacles or preconceived notions about medical practitioners or the illness. Thanks to the growing amount of medical information online, many people now use the Internet for health information, and 38% report that this influences their decision to see a doctor (Fox & Jones, 2009). Unfortunately, this is not always a good thing because individuals tend to do a poor job assessing the credibility of health information. For example, college-student participants reading online articles about HIV and syphilis rated a physician’s article and a college student’s article as equally credible if the participants said they were familiar with the health topic (Eastin, 2001). Credibility of health information often means how accurate or trustworthy the information is, and it can be influenced by irrelevant factors, such as the website’s design, logos, or the organization’s contact information (Freeman & Spyridakis, 2004). Similarly, many people post health questions on unmoderated forums online where anyone can respond, which allows for the possibility of inaccurate information being provided for serious medical conditions by unqualified individuals.
After individuals decide to seek care, there is also variability in the information they give their medical provider. Poor communication due to embarrassment or feeling rushed can influence the accuracy of the diagnosis and the effectiveness of the prescribed treatment. Similarly, there is variation following a visit to the doctor. While most individuals are tasked with a health recommendation (e.g., buying and using a medication appropriately, losing weight, or going to another expert), not everyone adheres to medical recommendations (Dunbar-Jacob & Mortimer-Stephens, 2001). For example, many individuals take medications inappropriately (e.g., stopping early or not filling prescriptions) or fail to change their behaviours (e.g., quitting smoking). Unfortunately, getting patients to follow medical orders is not as easy as one would think. For example, in one study, over one third of diabetic patients failed to get proper medical care that would prevent or slow down diabetes-related blindness (Schoenfeld, Greene, Wu, & Leske, 2001). Fortunately, as mobile technology improves, physicians now have the ability to monitor adherence and work to improve it (e.g., with pill bottles that monitor if they are opened at the right time). Even text messages are useful for improving treatment adherence and outcomes in depression, smoking cessation, and weight loss (Cole-Lewis, & Kershaw, 2010).
The future of health psychology
Much of the past medical research literature provides an incomplete picture of human health. “Health-care” is often “illness-care.” That is, it focuses on the management of symptoms and illnesses as they arise. As a result, in many developed countries, we are faced with several health epidemics that are difficult and costly to treat. These include obesity, diabetes, and cardiovascular disease, to name a few. Healthcare institutes have called for researchers to use the knowledge we have about risk factors to design effective interventions to reduce the prevalence of preventable illness. Additionally, there are a growing number of individuals across developed countries with multiple chronic illnesses or lasting disabilities, especially with older age. Addressing their needs and maintaining their quality of life will require skilled individuals who understand how to properly treat these populations. Health psychologists will be on the forefront of work in these areas.
With this focus on prevention, it is important that health psychologists move beyond studying risk (e.g., depression, stress, hostility, and low socioeconomic status) in isolation, and move toward studying factors that confer resilience and protection from disease. There is, fortunately, a growing interest in studying the positive factors that protect our health with evidence strongly indicating that people with higher positivity live longer, suffer fewer illnesses, and generally feel better (e.g., Diener & Chan, 2011; Pressman & Cohen, 2005; Richman, Kubzansky, Maselko, Kawachi, Choo, & Bauer, 2005). Martin Seligman (2008) has even proposed a field of “positive health” to specifically study those who exhibit above-average health — something we do not think about enough. By shifting some of the research focus to identifying and understanding these health-promoting factors, we may capitalize on this information to improve public health.
Innovative interventions to improve health are already in use and continue to be studied. With recent advances in technology, we are starting to see great strides made to improve health with the aid of computational tools. For example, there are hundreds of simple computer software applications that use email and text messages to send reminders to take medication, as well as mobile apps that allow us to monitor our exercise levels and food intake in the growing mobile-health, or m-health, field. These m-health applications can be used to raise health awareness, support treatment and compliance, and remotely collect data on a variety of outcomes. Also exciting are devices that allow us to monitor physiology in real time to better understand the stressful situations that raise blood pressure or heart rate. With advances like these, health psychologists will be able to serve the population better, learn more about health and health behaviour, and develop excellent health-improving strategies that could be specifically targeted to certain populations or individuals. These leaps in equipment development, partnered with growing health psychology knowledge and exciting advances in neuroscience and genetic research, will lead health researchers and practitioners into an exciting new time where, hopefully, we will understand more and more about how to keep people healthy.
Source: Adapted from Hooker and Pressman (2020).
Go online to learn techniques to improve your wellbeing
HeretoHelp (n.d.) is a project of the BC Partners for Mental Health and Substance Use Information. The website contains a wealth of information, resources, screening tests, and more designed to help people manage their mental health and substance use. Use their screening tests to evaluate your wellbeing.
“Stress Management: Health Tools” (2018) by Healthwise staff at HealthLinkBC has a number of useful resources if you would like to learn some specific stress management techniques such as breathing for relaxation, meditation, or time management.
Key Takeaways
- The biopsychosocial model of health posits that biology, psychology, and social factors are just as important in the development of disease as biological causes like germs and viruses.
- Several factors are known to contribute to resilience: the use of coping strategies, a sense of control and self-efficacy, good social relationships, a positive disposition and sense of optimism, and managing one’s stress.
- Health behaviours like sleeping enough and not smoking are protective against the effects of stress.
- The existence of computer software applications and other online applications is making it easier for people to engage in and monitor their positive health behaviours.
Exercises and Critical Thinking
- What psychological factors contribute to health?
- Which psychosocial constructs and behaviours might help protect us from the damaging effects of stress?
- What kinds of interventions might help to improve resilience? Who will these interventions help the most?
- How should doctors use research in health psychology when meeting with patients?
Congratulations on completing Chapter 12! Remember to go back to the section on Approach and Pedagogy near the beginning of the book to learn more about how to get the most out of reading and learning the material in this textbook.
Image Attributions
Figure 12.22. ALC Health Expo 5K Run by Adelphi Lab Center is used under a CC BY 2.0 license.
Figure 12.23. Used under a CC BY-NC-SA 4.0 license.
Figure 12.24. Sedum Rubrotinctum by JJ Harrison is used under a CC BY-SA 2.5 license.
Figure 12.25. Used under a CC BY-NC-SA 4.0 license.
Figure 12.26. Used under a CC BY-NC-SA 4.0 license.
Figure 12.27. WebMD Publishes Flu Risk Map with MapBox by Mapbox is used under a CC BY 2.0 license.
References
Adamson, J., Ben-Shlomo, Y., Chaturvedi, N., & Donovan, J. (2003). Ethnicity, socio-economic position and gender—Do they affect reported health-care seeking behaviour? Social Science & Medicine, 57(5), 895–904.
BC Partners for Mental Health and Substance Use Information. (n.d.). HeretoHelp. Retrieved from https://www.heretohelp.bc.ca
Belloc, N. B., & Breslow, L. (1972). Relationship of physical health status and health practices. Preventive Medicine, 1, 409–421.
Billings, A. G., & Moos, R. H. (1981). The role of coping responses and social resources in attenuating the stress of life events. Journal of Behavioral Medicine, 4, 139–157.
Breslow, L., & Enstrom, J. E. (1980). Persistence of health habits and their relationship to mortality. Preventive Medicine, 9, 469–483.
Briscoe, M. E. (1987). Why do people go to the doctor? Sex differences in the correlates of GP consultation. Social Science & Medicine, 25, 507–513.
Carver, C. S., Scheier, M. F., & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56, 267–283.
Cohen, S., & Herbert, T. B. (1996). Health psychology: Psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annual Review of Psychology, 47, 113–142.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357.
Cohen, S., Alper, C. M., Doyle, W. J., Treanor, J. J., & Turner, R. B. (2006). Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza A virus. Psychosomatic Medicine, 68, 809–815.
Cohen, S., Janicki-Deverts, D., & Miller, G. E. (2007). Psychological stress and disease. Journal of the American Medical Association, 298, 1685–1687.
Cohen, S., Tyrrell, D. A., & Smith, A. P. (1991). Psychological stress and susceptibility to the common cold. New England Journal of Medicine, 325, 606–612.
Cole-Lewis, H., & Kershaw, T. (2010). Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews, 32, 56–69.
Curcio, G., Ferrara, M., & De Gennaro, L. (2006). Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews, 10, 323–337.
Dickerson, S. S., & Kemeny, M. E. (2004). Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin, 130, 355–391.
Diener, E., & Chan, M. (2011). Happy people live longer: Subjective well-being contributes to health and longevity. Applied Psychology Health and Well-Being, 3(1), 1–43.
Dunbar-Jacob, J., & Mortimer-Stephens, M. (2001). Treatment adherence in chronic disease. Journal of Clinical Epidemiology, 54(12), S57–S60
Eastin, M. S. (2001). Credibility assessments of online health information: The effects of source expertise and knowledge of content. Journal of Computer Mediated Communication, 6.
Fox, S., & Jones, S. (2009). The social life of health information. Pew Internet and American Life Project, California HealthCare Foundation. Retrieved from http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx
Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218–226.
Freeman, K. S., & Spyridakis, J. H. (2004). An examination of factors that affect the credibility of online health information. Technical Communication, 51, 239–263.
Friedman, M., & Rosenman, R. (1959). Association of specific overt behaviour pattern with blood and cardiovascular findings. Journal of the American Medical Association, 169, 1286–1296.
Glass, D. C., & Singer, J. E. (1972). Behavioral aftereffects of unpredictable and uncontrollable aversive events: Although subjects were able to adapt to loud noise and other stressors in laboratory experiments, they clearly demonstrated adverse aftereffects. American Scientist, 60, 457–465.
Healthwise Staff. (2018). Stress management. HealthLinkBC. Retrieved from https://www.healthlinkbc.ca/health-topics/rlxsk#rlxsk-HealthTools
Herman-Stabl, M. A., Stemmler, M., & Petersen, A. C. (1995). Approach and avoidant coping: Implications for adolescent mental health. Journal of Youth and Adolescence, 24, 649–665.
Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7(7), e1000316.
Hooker, E., & Pressman, S. (2020). The healthy life. In R. Biswas-Diener & E. Diener (Eds.), Noba textbook series: Psychology. Champaign, IL: DEF. Retrieved from http://noba.to/4tm85z2x
House, J. S., Landis, K. R., & Umberson, D. (1988). Social relationships and health. Science, 241, 540–545.
Iribarren, C., Sidney, S., Bild, D. E., Liu, K., Markovitz, J. H., Roseman, J. M., & Matthews, K. (2000). Association of hostility with coronary artery calcification in young adults. Journal of the American Medical Association, 283, 2546–2551.
Kubzansky, L. D., Sparrow, D., Vokonas, P., & Kawachi, I. (2001). Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosomatic Medicine, 63, 910–916.
Matthews, K. A., Glass, D. C., Rosenman, R. H., & Bortner, R. W. (1977). Competitive drive, pattern A, and coronary heart disease: A further analysis of some data from the Western Collaborative Group Study. Journal of Chronic Diseases, 30, 489–498.
Meara, E., White, C., & Cutler, D. M. (2004). Trends in medical spending by age, 1963–2000. Health Affairs, 23, 176–183.
Miller, T. Q., Smith, T. W., Turner, C. W., Guijarro, M. L., & Hallet, A. J. (1996). Meta-analytic review of research on hostility and physical health. Psychological Bulletin, 119, 322–348.
Moravec, C. S. (2008). Biofeedback therapy in cardiovascular disease: rationale and research overview. Cleveland Clinic Journal of Medicine, 75, S35–S38.
Nes, L. S., & Segerstrom, S. C. (2006). Dispositional optimism and coping: A meta-analytic review. Personality and Social Psychology Review, 10, 235–251.
Oaten, M., & Cheng, K. (2005). Academic examination stress impairs self–control. Journal of Social and Clinical Psychology, 24(2), 254–279.
O’Leary, A. (1985). Self-efficacy and health. Behaviour Research and Therapy, 23, 437–451.
Patel, C., Marmot, M. G., & Terry, D. J. (1981). Controlled trial of biofeedback-aided behavioural methods in reducing mild hypertension. British Medical Journal (Clinical Research Ed.), 282(6281), 2005–2008.
Pressman, S. D., & Cohen, S. (2005). Does positive affect influence health? Psychological Bulletin, 131, 925–971.
Pressman, S. D., Gallagher, M. W., & Lopez, S. J. (2013). Is the emotion-health connection a “first-world problem”? Psychological Science, 24, 544–549.
Richman, L. S., Kubzansky, L., Maselko, J., Kawachi, I., Choo, P., & Bauer, M. (2005). Positive emotion and health: Going beyond the negative. Health Psychology, 24, 422–429.
Rodin, J., & Langer, E. J. (1977). Long-term effects of a control-relevant intervention with the institutionalized aged. Journal of Personality and Social Psychology, 35, 897–902.
Rutter, M. (1985). Resilience in the face of adversity. British Journal of Psychiatry, 147, 598–611.
Salmon, P. (2001). Effects of physical exercise on anxiety, depression, and sensitivity to stress: A unifying theory. Clinical Psychology Review, 21(1), 33–61.
Scheier, M. F., & Carver, C. S. (1985). Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology, 4, 219–247.
Schoenfeld, E. R., Greene, J. M., Wu, S. Y., & Leske, M. C. (2001). Patterns of adherence to diabetes vision care guidelines: Baseline findings from the Diabetic Retinopathy Awareness Program. Ophthalmology, 108, 563–571.
Schulz, R., & Hanusa, B. H. (1978). Long-term effects of control and predictability-enhancing interventions: Findings and ethical issues. Journal of Personality and Social Psychology, 36, 1194–1202.
Segerstrom, S. C., Taylor, S. E., Kemeny, M. E., & Fahey, J. L. (1998). Optimism is associated with mood, coping, and immune change in response to stress. Journal of Personality and Social Psychology, 74, 1646–1655.
Seligman, M. E. P. (2008). Positive health. Applied Psychology, 57, 3–18.
Sieber, W. J., Rodin, J., Larson, L., Ortega, S., Cummings, N., Levy, S., … Herberman, R. (1992). Modulation of human natural killer cell activity by exposure to uncontrollable stress. Brain, Behavior, and Immunity, 6, 141–156.
Spiegel, D., Kraemer, H., Bloom, J., & Gottheil, E. (1989). Effect of psychosocial treatment on survival of patients with metastatic breast cancer. The Lancet, 334, 888–891.
Statistics Canada. (2019). Health characteristics, annual estimates (Table 13-10-0096-01). Retrieved from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009601
Taylor, S. E. (2012) Health psychology (8th ed.). New York, NY: McGraw-Hill.
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107, 411–429.
Wallston, B. S., & Wallston, K. A. (1978). Locus of control and health: a review of the literature. Health Education & Behavior, 6, 107–117.
World Health Organization. (1946). Preamble to the Constitution of the World Health Organization. Retrieved from http://www.who.int/about/definition/en/print.html
World Health Organization. (2013). Cardiovascular diseases. Retrieved from http://www.who.int/mediacentre/factsheets/fs317/en/index.html

